Xenotransplantation
The Problem
There are 3 types of transplants. ISO-transplantation which living cells, tissues or organs are transplanted from a donor to a genetically identical recipient (such as an identical twin). ALLO-transplantation involves transplanting living cells, tissues or organs from one human to another (current practice), and XENO-transplantation which is the transplantation of living cells, tissues or organs from one species to another.
Both Isotransplantation and Allotransplantation are possible today, but there aren’t enough donor organs to satisfy the demand. That has resulted in a transplant waiting list. Approximately 17 people die each day while waiting for a donor to become available. This is why researchers have pursued xenotransplantation by creating a new source of donor organs from animals. Makana Therapeutics is uniquely positioned to achieve this goal.
Why do Transplants Fail?
The human immune system protects individuals from substances that may be harmful, such as germs, poisons, and sometimes, cancer cells. These harmful substances are covered in “antigens” which coat the surface of their cells. As soon as these antigens enter the body, the immune system recognizes that they are “foreign”, and it produces antibodies that attack the foreign cells. In transplantation, this phenomenon is called Antibody Mediated Rejection (AMR). There are 2 degrees of AMR, either acute or hyperacute. Most transplanted tissues experience some form of acute rejection, but this is usually a manageable condition because of pre-transplant tissue matching. However, when the HLA between donor and recipient are mismatched, that prompts a hyperacute rejection episode. During hyperacute rejection, the transplanted organ can immediately sustain severe damage, and it must be removed.
Early attempts at xenotransplantation were always met with episodes of hyperacute rejection because little was known about the specific antigens that pigs expressed on their cell surface. As the body of knowledge grew in allotransplantation, scientists better understood the pathways of antibody mediated rejection in xenografts. Scientists discovered 3 known xeno-antigens that needed to be removed from the pig genome, but genetic engineering technology was in its infancy. Then, in 2012, CRISPR-Cas9 was introduced to the world. Scientists were able to make multiple genome modifications in a very short time. This invention greatly accelerated engineering efforts and reinvigorated xenotransplantation research.
The Makana team members collectively have spent more than a three decades researching xenotransplantation and developing the expertise necessary to deliver world-class results. They have chosen to focus efforts on 3 key areas which will bring xenotransplantation to the clinic.
Dr. Tector and the team at Makana have spent more than a decade developing leading world class expertise in three critical areas needed to make xenotransplantation a future option for patients:
Genetic Engineering
Proprietary Transplant
Crossmatch Assays
Animal Husbandry and
Advanced Reproduction
of Pigs
Genetic Engineering
The Makana lab discovered the 3 key xenoantigens that pigs have on the surface of their cells, and have knocked out” the genes in the pig that cause the cells to express these xenoantigens. Eliminating these xenoantigens has been shown to evade pre-existing and de novo antibodies that are the cause of organ rejection in humans. This baseline genetic makeup is called the “Triple Knock Out” or TKO. Here are the key Xenoantigens that Makana organs lack:
α-1,3-galactosyltransferase
knockout (GGTA1-KO)
β-1,4-N-acetyl-galactosaminyl
transferase2 knockout
(B4GALNT2-KO)
Cytidine monophosphate-N-acetylneuraminic
acid hydroxylase knockout
(CMAH-KO)
Makana’s preclinical work further suggests that continued deletion of xenoantigens will be a successful approach to overcoming the later stages of antibody mediated rejection. Makana’s preclinical data shows >60% 400-day survival rates preclinically, and recipients surviving more than 3 years confirms this.
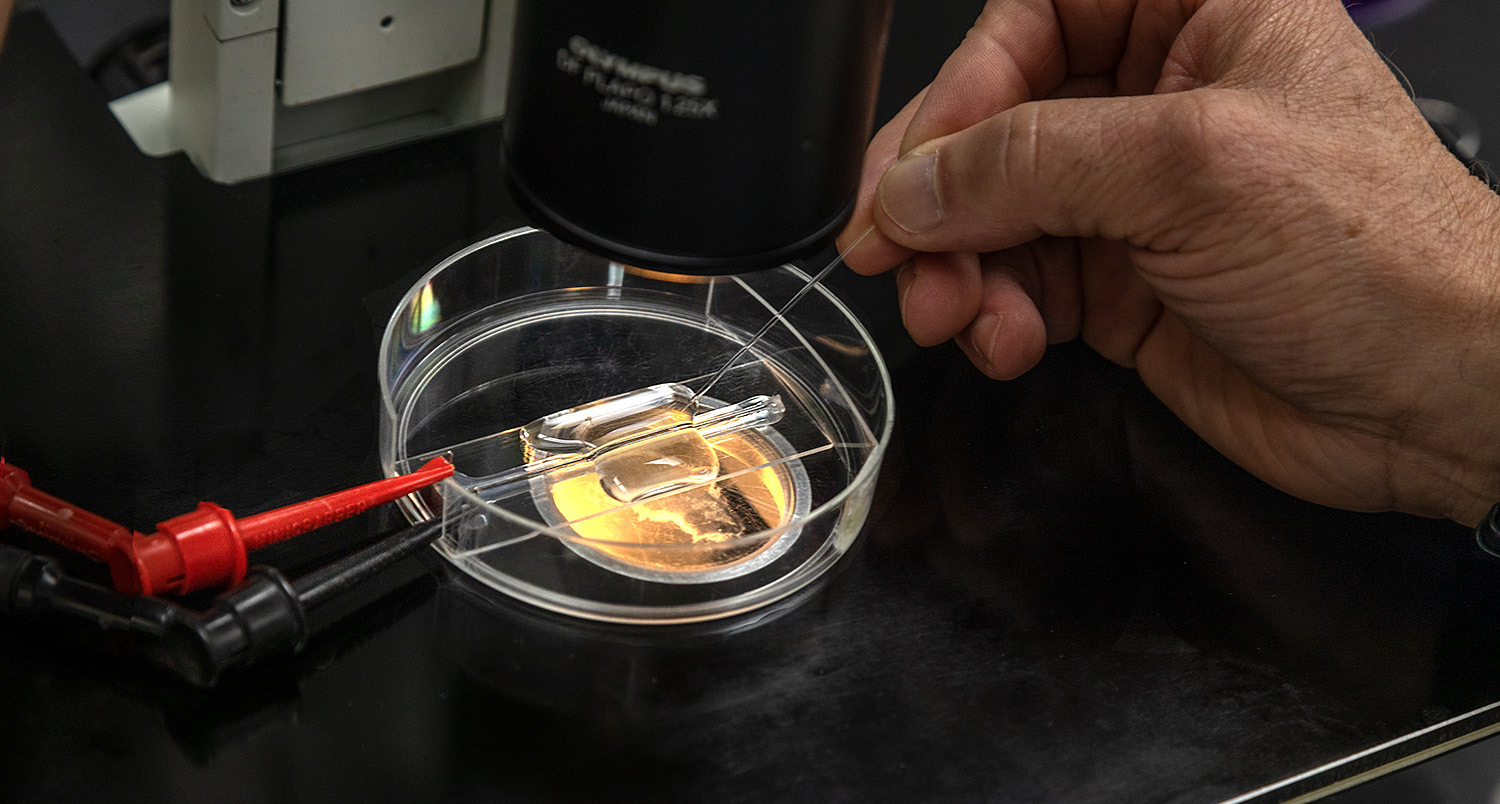
Proprietary Cross Match Assay
Makana’s proprietary crossmatch assays will identify patients without pre-existing donor-specific antibodies. This, in turn, will reduce the likelihood of antibody mediated rejection.
Histocompatibility testing with xenoantigen deficient pig cells and human serum from patients on the kidney transplant waitlist suggest that 30% of human patients will have no detectable antibodies against xenoantigen deficient tissues; another 40% of patients will accept xenoantigen deficient tissue with available pre-transplant treatment. In Makana pre-clinical studies, recipients with low anti-pig antibodies achieved the best survival following transplant.
%
xenoantigen deficient tissues
+
%
pre-transplant treatment
=
%
Animal Husbandry
Makana uses the latest reproductive methods and technology to reliably produce healthy, gene-edited animals on a commercial scale. This allows for the highest quality “clinical grade” animal production standards in the industry.
