Kidney
What are Kidneys?
The kidneys, each just the size of a human fist, filter all the blood in a person’s body every 30 minutes. They work hard to remove wastes, toxins, and excess fluid. They also help control blood pressure, stimulate production of red blood cells, keep your bones healthy, and regulate blood chemicals that are essential to life.

What is Chronic Kidney Disease (CKD)?
CKD occurs when the kidneys are damaged and lose their ability to filter the blood. In the early stages of the disease, most people do not have symptoms. But as kidney disease gets worse, wastes can build up in a person’s blood and make them feel sick. Because kidneys are vital to so many of the body’s functions, kidney disease also increases the risk of having heart and blood vessel disease. While these problems may happen slowly and without symptoms, they can lead to kidney failure, which can appear without warning.
Kidney disease causes more deaths than breast cancer or prostate cancer in the U.S.
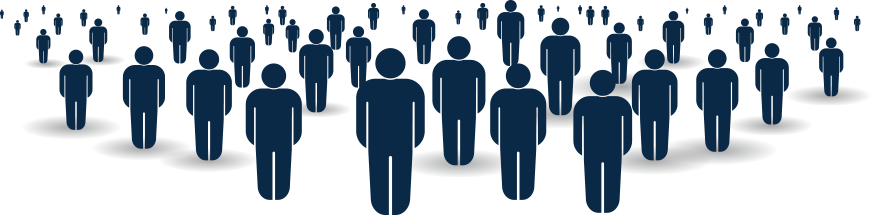
Its estimated that Chronic Kidney Disease (CKD) affects more than 1 in 7 US Adults, or
OR 37 MILLION PEOPLE
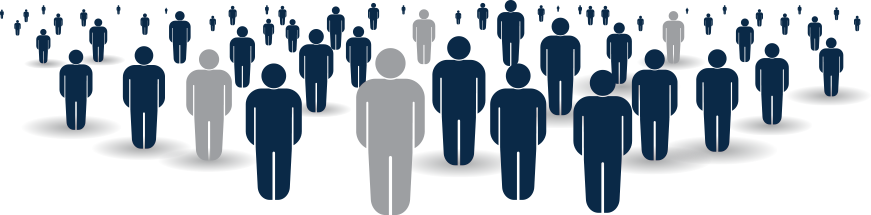
1 in 3 adults in the U.S. are at risk for kidney disease.
APPROX. 80 MILLION PEOPLE
Kidney disease is a leading cause of death in the U.S.
What are the main causes of chronic kidney disease?
Diabetes and high blood pressure, or hypertension, are responsible for two-thirds of chronic kidney disease cases.
Diabetes: Diabetes occurs when your blood sugar remains too high. Over time, unmanaged blood sugar can cause damage to many organs in your body, including the kidneys and heart and blood vessels, nerves, and eyes.
High blood pressure: High blood pressure occurs when your blood pressure against the walls of your blood vessels increases. If uncontrolled or poorly controlled, high blood pressure can be a leading cause of heart attacks, strokes, and chronic kidney disease. Also, chronic kidney disease can cause high blood pressure.
Other conditions that can lead to kidney disease:
Glomerulonephritis: Glomerulonephritis is a group of diseases that cause inflammation and damage the kidney’s filtering units. These disorders are the third most common type of kidney disease.
Inherited diseases: Polycystic kidney disease, or PKD, is a common inherited disease that causes large cysts to form in the kidneys and damage the surrounding tissue.
Kidney and urinary tract abnormalities before birth: Malformations that occur as a baby develops in its mother’s womb. For example, a narrowing may occur that prevents normal outflow of urine and causes urine to flow back up to the kidney. This causes infections and may damage the kidneys.
Autoimmune diseases: When the body’s defense system, the immune system, turns against the body, it’s called an autoimmune disease. Lupus nephritis is one such autoimmune disease that results in inflammation (swelling or scarring) of the small blood vessels that filter wastes in your kidney.
Other causes: Obstructions caused by kidney stones or tumors can cause kidney damage. An enlarged prostate gland in men or repeated urinary infections can also cause kidney damage.
What is End-stage Renal Disease (ESRD)?
End-stage renal disease, or kidney failure, occurs when chronic kidney disease reaches a critical point where the Kidneys are no longer able to filter wastes and excess fluids from your blood. When this happens, dangerous levels of fluid, electrolytes and toxins can build up in your body, and make you very ill. It can also cause damage to other organs in your body and will lead to death if left untreated.
12 people die every day while waiting for a kidney transplant



How is Kidney Failure treated?
Treatment comparison: dialysis or transplant?
Dialysis is a life sustaining therapy, but many complications arise over time. Patients treated with hemodialysis (HD) may experience acute complications including cardiac arrhythmias, infection, vessel occlusion, hypotension, hypertension, dialysis disequilibrium syndrome, allergic reactions, air embolism, bleeding, and seizures. These acute complications are more rare due to advances in the equipment safety and staff training at dialysis centers. However, there are regular symptoms that patients experience from dialysis such as fatigue, cramps, nausea, vomiting, and headaches. These symptoms can be debilitating for patients and can cause patients to quit dialysis altogether. The 5-year survival rate for those on dialysis is around 50%. The benefit to dialysis, is that its readily available to all, but the drawback is poor quality of life, poor long-term survival, and higher overall cost.
Kidney Transplant is the best therapy for ESRD, and the outcomes are much better than dialysis. According to the national Organ Procurement and Transplantation Network, the success rate of kidney transplants are listed below:
Success rate after a kidney transplant
with a living-donor kidney
Success rate after transplant with
a deceased-donor kidney
%
1 YEAR
%
5 YEAR
%
1 YEAR
%
5 YEAR
Kidney Disease Resources
Please visit these organizations for more information on kidney disease and how to become an organ donor:







